Under the Microscope: New research zeroes in on persistent tuberculosis
A new study from the University of Toronto aims to a unravel the mystery of why some tuberculosis cases fail to respond to medical treatment.
The interdisciplinary collaboration between U of T Mississauga physicist Joshua Milstein and biomedical engineer Jonathan Rocheleau of U of T’s Institute of Biomaterials and Biomedical Engineering was recently awarded funding through U of T’s XSeed Funding Program, an initiative that offers new opportunities for collaboration and partnerships with the Faculty of Applied Science & Engineering. Milstein and Rocheleau will share $60,000 per year for a two-year pilot study of antibiotic-resistant tuberculosis.
Tuberculosis is one of the world’s most deadly diseases, infecting about 10 million people and killing 1.3 million people in 2017. Contagious Mycobacterium tuberculosis spreads through the air and typically attacks the lungs of those infected. Left untreated, it can be fatal, however the disease is often treatable with an intensive months-long regime of antibiotic medication.
Sometimes, however, the antibiotics don’t work. Some bacterium, known as “persistors,” slow down in metabolic activity and fail to ingest the disease-killing antibiotics. Those bacteria may continue to live on in the lungs, and have the potential to reanimate in the future to cause a new infection.
“We want to understand why some cells become persistors so we can target ways to kill those cells,” says Milstein, an associate professor with UTM’s Department of Chemical & Physical Sciences. His research uses cutting-edge microscopy to understand the inner workings of bacteria and viruses. “Persistors are hard to study because there are only a few of them in a population. If we had a measure of different aspects of metabolic rates in these cells, we might be able to see how changes in metabolism lead to these persistors.”
That’s where Rocheleau’s expertise comes in. Rocheleau’s main research uses nanotechnology to study the early stages of Type 2 diabetes, using genetically encoded sensors that cause a cell to glow whenever a protein or gene is in use. This technique will be applied to bacteria grown in the Milstein lab to better understand the behaviour of individual bacterium that may become persistors.
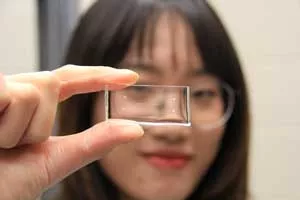
The team will initially study non-infectious E. coli bacteria which will be grown on special slides manufactured in the Milstein Lab. Each slide can host hundreds of tiny chambers which mimic pockets in the lung. Viewed through the lab’s high-powered microscopes, the glowing green bacterium jostle together single-file in a chamber just five microns high and one micron deep, allowing the researchers to see individual bacterium grow and divide in real time. “We can easily add antibiotics or small molecules into the chambers and see how the colonies behave,” Milstein says. “If we want to measure how a protein might respond to antibiotics, we would connect that to a glowing sensor tuned to whatever molecule we’re looking for inside the cell. It’s an indicator of the genetic response of the cells.”
“This project brings together things that each lab can’t do on its own,” Milstein says. “We can combine these measures of metabolism with microscopy to understand how cells become persistent, and figure out ways to target them with different antibiotics or drugs.”
