UTM prof and clinical education partner deliver vital training to grad students during pandemic
Surgical observation very nearly didn't happen this past semester for first-year Master of Science in Biomedical Communications students.
To preserve resources such as ICU beds for COVID patients, on April 7, 2021, the Ontario government ordered hospitals to postpone all elective and non-emergency surgeries. Surgeries that could take place were restricted to essential personnel only.
Fortunately, a Biomedical Communications (BMC) faculty member was able to leverage the close relationship between the BMC program and its clinical educational partner at Mount Sinai Hospital to create a surgical observation opportunity exclusively for BMC graduate students.
COVID's third wave
"We had moved surgical illustration from January to the spring thinking surely the students will be able to enter the operating room by then. Then the third wave hit and it was out of the question for any non-essential personnel to be in the OR," says Shelley Wall, associate professor in UTM's Master of Science in Biomedical Communications program.
Wall and her colleague Lisa Satterthwaite, the senior manager of the University of Toronto’s Surgical Skills Centre at Mount Sinai Hospital, decided to mount a dedicated session exclusively for the BMC graduate students.
The Surgical Skills Centre provides a laboratory setting where surgeons, medical students, residents, fellows and physicians can learn and practice basic and complex surgical and medical procedures on cadavers, organ tissue, analog or digital simulators.
"I contacted a few surgeons who spoke with their residents to see who would be interested. We had a response of five residents who volunteered to come in and do dissections on cadaveric tissue provided by the Department of Anatomy," says Satterthwaite. Anatomy has also struggled under COVID with donations having been very much reduced, she says. "They've had a tough time of it, but they were more than willing to help us out with this program."
To prepare for surgical observation, Wall lectured the students on the basics of surgical procedure. She also instructed them on visual narrative to give them a sense of what to look for while observing procedures, and what questions to ask.
Orthopaedic surgery observation
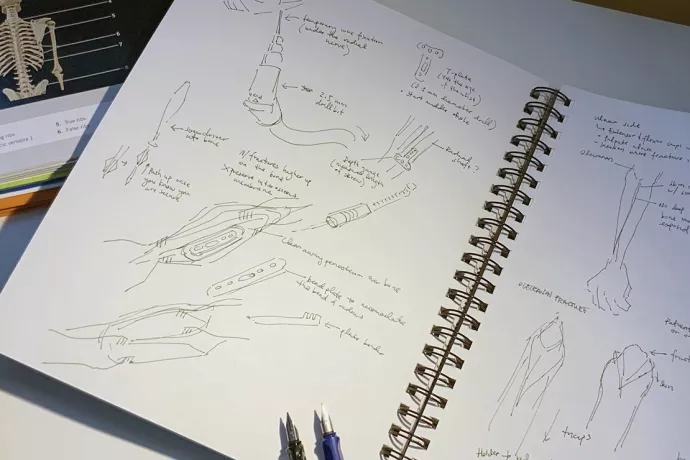
On May 6, the first-year biomedical communications students attended orthopaedic trauma surgery in the Surgical Skills Centre’s training theatre. They observed techniques such as plating of fractures, fasciotomies, suturing wound closures and dissections.
The observership differed from what the students might have experienced in the OR.
"Cadaveric material is obviously not the same as actually seeing live tissue in a surgical field. There's also a lot of instrumentation or procedures such as suction or cautery that they did not see," says Wall. But neither did the students have to worry about entering the surgical field or interrupting the surgeon. "The residents were very happy to pause and explain all the underlying relevant anatomy."
Speed sketching
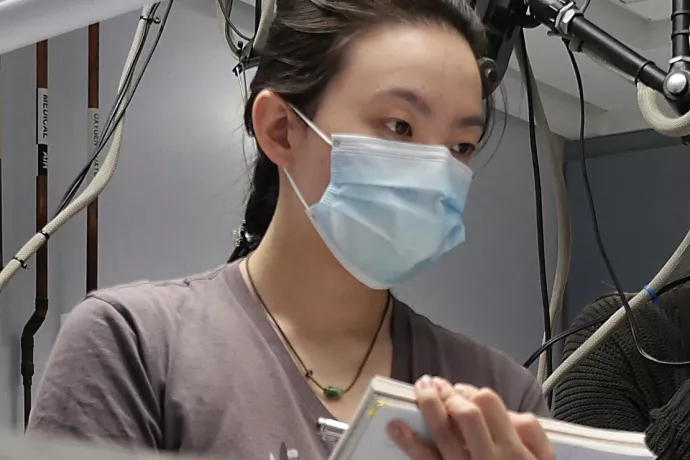
Aimy Meng Yu Wang, a biomedical communications graduate student, compared sketching the surgical demonstrations to figure drawing.
"We only had a short amount of time to capture a movement, a sequence, a set of steps–so every stroke had to count," says Wang. "It was great that we were in the SSC because we could ask the surgeons questions directly. This would have been much more difficult to do in the OR with a patient on the operating table."
Also unique to the session was that the students were able to participate.
"I've never experienced orthopaedic surgery before, so the power tools were a shock. But it was really exciting when we had the chance to try to drill into the bone and fix plates into it ourselves. It became truly hands-on," Wang says.
Surgical illustration skills are transferable to all aspects of medical illustration and animation, says Shelley Wall. "Students have to bring to bear all the anatomical and procedural knowledge they are gaining. This experience crystallizes what needs to be done to tell a good visual story."
Space permitting, Lisa Satterthwaite hopes that there may be future opportunities for the biomedical communications students to observe other surgical training sessions. "Because COVID has reduced our ability to deliver education, we were thrilled from the skills laboratory side to be able to offer this opportunity," she says.
